Making Time Matter: A Palliative Perspective on Presence, Connection, and Legacy

In palliative care, time can be understood in two ways. Clock time – the hours and minutes measured in schedules and calendars, and temporality – how people experience their time. For those living with serious illnesses, time becomes both fragile and profound. Caregivers and families who walk alongside them may feel this too. As explored […]
Reflections from the 4th International Research Seminar: EAPC Reference Group on Public Health and Palliative Care, University of Victoria June 17-19 2025

By: Dawn Elston – Life and Death MattersFeatured Photo: Drs Leah Norgrove, Ambrose Marsh, Fraser Black, and Kath Murray and Coby Tschanz This year’s European Association of Palliative Care 4th International Research Seminar was held at the University of Victoria! The seminar focused on “Innovating Care: Research and Action for Public Health and Palliative Care”. […]
Honouring Compassion in Action: Myke Dyer Wins the 2025 Frances Montgomery PSW Award
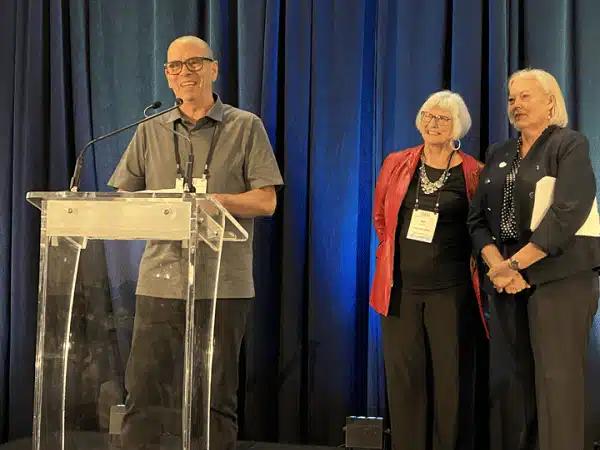
Life and Death Matters is proud to announce that Myke Dyer, a truly exceptional Personal Support Worker (PSW) at Hospice Georgian Triangle, is the 2025 recipient of the Frances Montgomery PSW Award. Sponsored by Life and Death Matters and presented at the Hospice Palliative Care Ontario annual conference (HPCO), this annual award celebrates excellence in […]
Grief and bereavement in the 2SLGBTQ+ community: exploring challenges and resilience
By Geoff Straw, M.A. Registered Psychotherapist (Ontario), Registered Clinical Counsellor (British Columbia) “I learned that different meant many things: freedom, oppression, celebration, sadness, responsibility, hiding, protesting, sharing, but most of all being true to one’s self no matter the price.”Liza Minelli Pride: A Time for Celebration and Advocacy As many communities across Canada prepare to […]

